PGS Testing Risks and Benefits: What to Know

PGS Testing Risks and Benefits
Reproductive technology is advancing rapidly, and Preimplantation Genetic Screening (PGS) is now a game-changer in IVF treatments. This advanced screening method helps intended parents select the healthiest embryos, significantly increasing the chances of a successful pregnancy and reducing the risk of genetic disorders.
However, while PGS testing offers many benefits, such as higher implantation success rates and a lower chance of miscarriage, it also has potential risks.
- Book an online appointment: Get a free online consultation.
- Call\W:+91-8800481100 Email:neelam@ivfconceptions.com
Some concerns include the possibility of embryo damage during testing, false positives or negatives, and the fact that PGS does not screen for all genetic conditions.
For couples considering PGS testing in IVF, understanding the risks and benefits is crucial for making an informed decision. Consulting with a fertility specialist can help determine if genetic screening for embryos is the right choice for your fertility journey.
Key Takeaways
- PGS testing has a less than 1% risk of damaging an embryo during cell extraction.
- PGS is 97% accurate at finding if an embryo has the right number of chromosomes.
- About 5% of embryos might have cells that are too poor for testing after cell extraction.
- PGS can only work on Day 5 embryos that are in good quality, leaving out those that aren’t.
- PGS doesn’t check for genetic diseases or tell you about specific genetic conditions.
More Resources to Read:
Surrogacy Guide for Surrogate Mothers
Surrogacy Guide for Intended Parents
How does the surrogacy process work
Understanding PGS Testing and Its Procedure
PGS testing, also known as Preimplantation Genetic Screening, is a procedure that has rapidly gained popularity in the field of reproductive medicine. It involves testing embryos for genetic abnormalities before they are transferred into the womb during the process of in-vitro fertilization (IVF). PGS testing aims to identify embryos that have a higher chance of implanting successfully and results in the birth of a healthy baby.
One of the main benefits of PGS testing is its ability to detect chromosomal abnormalities in embryos. By identifying genetic errors that can lead to birth defects or miscarriages, PGS testing provides couples with valuable information that can help them make informed decisions about their treatment options. The diagnostic accuracy of PGS testing has significantly improved over the years, making it a reliable tool for identifying abnormal embryos.
Like any medical procedure, PGS testing also carries certain risks. The most common risk associated with PGS testing is the possibility of misdiagnosis. Although advancements in technology have improved the accuracy of PGS testing, there is still a small chance of false positives or false negatives. It is important for couples to understand the limitations of PGS testing and discuss the potential risks with their healthcare provider.
Preimplantation genetic screening (PGS), also known as preimplantation genetic testing for aneuploidy (PGT-A), is a key technique in IVF. It checks the chromosomes of embryos. The main aim is to find embryos with the right number of chromosomes, called euploid embryos. These embryos are more likely to implant well and lead to a healthy pregnancy.
What is PGS Testing (PGT-A)?
PGT-A looks for extra or missing chromosomes in embryos. Wrong chromosome numbers can cause implantation failure, miscarriage, or health problems later. A normal embryo has 46 chromosomes, half from mom and half from dad.
How is PGS Testing Performed?
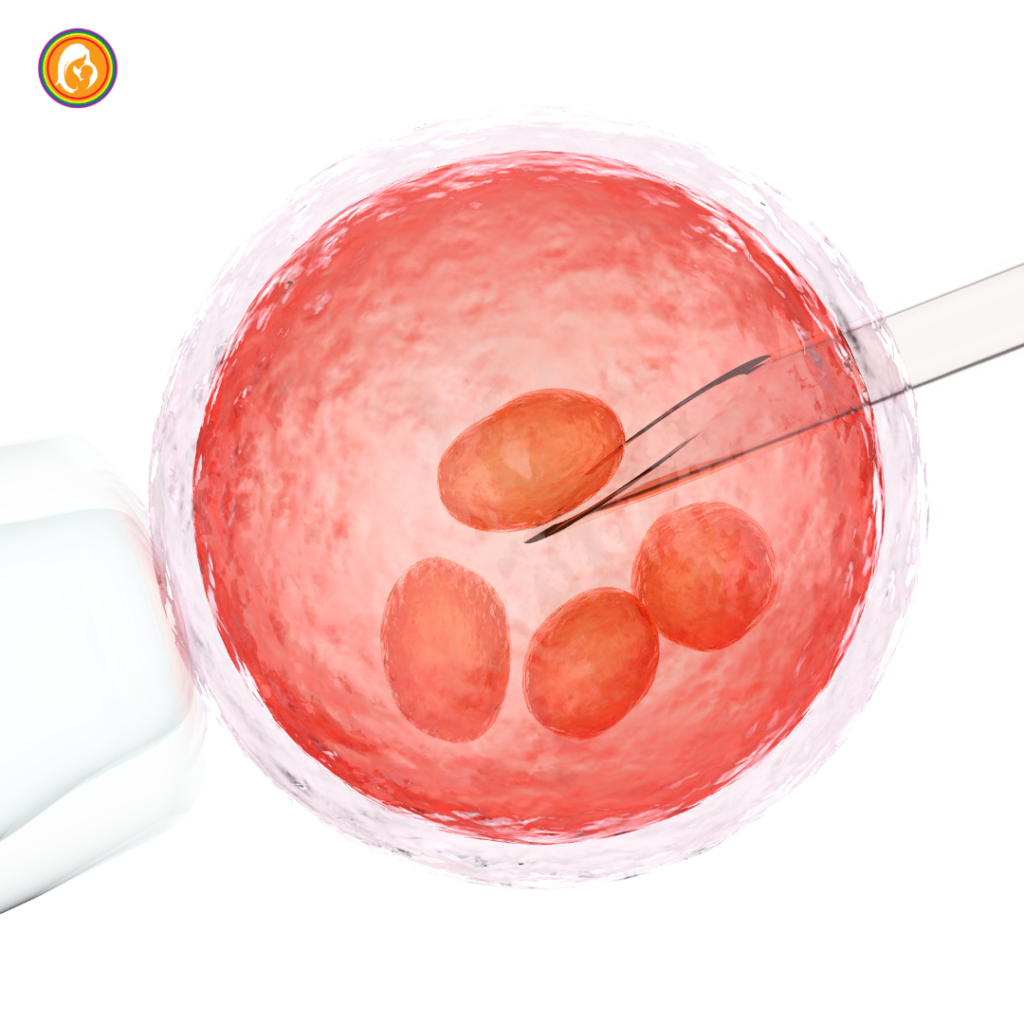
The process starts with taking a small cell sample from the embryo at the blastocyst stage. This is done with a laser to avoid harming the embryo. Then, the genetic material is checked to see if the embryo has the right number of chromosomes. If it does, it’s called euploid; if not, aneuploid.
| Procedure | Description |
| Embryo Biopsy | A small sample of cells is removed from the embryo, typically during the blastocyst stage, using a laser to minimize disruption. |
| Chromosomal Analysis | The genetic material collected from the embryo is analyzed to determine its chromosomal status, categorizing it as either euploid (normal) or aneuploid (abnormal). |
| Embryo Selection | Based on the chromosomal analysis, the healthiest euploid embryos are selected for transfer or cryopreservation, with the goal of improving the success rate of the IVF process. |
PGS testing helps pick out the healthiest embryos. This increases the chance of a successful pregnancy and lowers the risk of miscarriage or chromosomal abnormalities in the child.
Does PGS Testing Harm the Embryo?
Many people worry if PGS (preimplantation genetic screening) testing hurts the embryo. This worry has sparked a lot of research and debate among fertility experts.
Potential Risks of Embryo Biopsy
Removing a few cells from the embryo for tests might affect its growth and ability to implant. Studies found that biopsying at the cleavage stage (Day 3) can lower implantation rates. On the other hand, biopsying at the blastocyst stage (Day 5) has a smaller effect.
Factors Affecting Embryo Damage During Biopsy
The skill of the embryologist doing the biopsy matters too. Big biopsies are linked to lower live birth rates. This shows that how the embryologist does the biopsy can change the results.
Also, the quality of the lab and its methods can affect how accurate PGS tests are. Some labs have better live birth rates than others. This means picking a trusted and skilled PGS testing lab is key.
“PGT-A testing has been shown to improve the odds of a live birth in patients as young as age 35, indicating potential benefits for younger patients in embryo selection.”
Even with concerns, PGS testing has big benefits, especially for older women. Women over 35 see better live birth rates and fewer miscarriages with PGS testing. Yet, deciding on PGS testing should be talked over with a fertility expert. It’s important to weigh the risks and benefits for you.
PGS Testing risks and benefits
Benefits: Improved Success Rates and Reduced Miscarriage Risk
PGS testing can boost IVF success rates and lower miscarriage risk. It aims to transfer only healthy embryos, increasing the chance of a successful pregnancy. 30% of embryos in women under 35 are abnormal, rising to 85% in women over 42. PGS helps avoid these abnormal embryos.
It also cuts down on multiple pregnancies by focusing on one healthy embryo. This reduces twin births. PGS testing makes successful pregnancies more likely than without it.
Limitations: Accuracy Concerns and Mosaic Embryos
PGS testing has its downsides. Next-Generation Sequencing (NGS) is the most precise method now. Older methods were less accurate, sometimes leading to wrong embryo choices.
Another issue is mosaic embryos, which mix normal and abnormal cells. These embryos are hard to diagnose but might still lead to healthy babies. Researchers are working to improve PGS testing to tackle these challenges.
| Benefit | Limitation |
| Improved IVF success rates | Accuracy concerns with older testing methods |
| Reduced miscarriage risk | Difficulties in diagnosing mosaic embryos |
| Decreased incidence of multiple pregnancies | Ongoing research to address limitations |
Overcoming Challenges with PGS Testing
PGS testing has made big strides, but there are still big challenges to beat. One major challenge is getting embryos to the blastocyst stage for biopsy. This stage is needed for the test.
Making Euploid Embryos: Blastocyst Development and Aneuploidy Rates
Getting embryos to the blastocyst stage is key for PGS testing. It lets us take more cells for biopsy. Studies show better implantation rates and fewer miscarriages with PGS on blastocyst embryos. But, not all embryos make it to the blastocyst stage. And even those that do might have chromosomal issues, or aneuploidy.
Aneuploidy means having the wrong number of chromosomes in IVF embryos. This happens in 40% to 80% of embryos, based on the mother’s age. PGS testing tries to pick the euploid embryos, those with the right number of chromosomes. This can help increase the chances of a successful pregnancy.
| Study | Findings |
| 2003 study | Improved implantation after preimplantation genetic diagnosis of aneuploidy |
| 2007 study | Reduced spontaneous abortion and increased live birth rates after preimplantation genetic diagnosis for advanced maternal age |
| 2008 study | Preimplantation genetic screening in women of advanced maternal age caused a decrease in the clinical pregnancy rate |
Research and new tech are working to make embryonic biopsy safer and more effective in ART. They aim to improve the creation of euploid embryos too.
Pros and cons of PGS
Deciding on preimplantation genetic screening (PGS) testing means looking at both the good and the bad. PGS, or preimplantation genetic testing for aneuploidy (PGT-A), checks embryos for chromosomal issues before transferring them. This can help improve pregnancy success and lower miscarriage risks.
Advantages of PGS Testing:
- Improved success rates: PGS helps pick healthy embryos, boosting the chance of a successful pregnancy and cutting down on embryo transfers.
- Reduced miscarriage risk: Choosing embryos with the right number of chromosomes lowers the risk of miscarriage.
- Identification of genetic disorders: PGS can spot genetic conditions like cystic fibrosis, helping in making informed choices and picking healthy embryos.
Disadvantages of PGS Testing:
- Cost-effectiveness: PGS costs about $4,000 on average, which might be too high for some patients.
- Accuracy concerns: PGS is very accurate but can have false positives or negatives, especially with mosaic embryos.
- Ethical considerations: Some people worry about the ethics of genetic testing and choosing certain embryos over others.
Choosing PGS testing should be a talk with a fertility expert. Think about your own situation, goals, and worries. Knowing the good and bad of PGS helps you make a choice that fits your needs.
“PGS can be a valuable tool in assisted reproductive technology, but it’s important for patients to have a comprehensive understanding of the potential benefits and limitations before making a decision.”
More Resources to Read:
Infertility Treatment and Surrogacy Process
9 Factors To Improve IVF Pregnancy Rate
International Surrogacy Options Worldwide
Surrogacy Guide for Surrogate Mothers
Conclusion
Preimplantation genetic screening (PGS), also known as PGT-A, is a complex reproductive technology. It aims to improve IVF success by picking chromosomally normal embryos for transfer. While it has potential benefits, like lowering miscarriage risk for some, it also has big limitations and risks.
The choice to use PGS should be made with a detailed talk with a fertility expert. This should consider the patient’s unique situation, goals, and what they prefer. Patients need to know about PGS’s accuracy, the effect of mosaicism, and the emotional and financial impacts.
By making an informed choice about fertility treatments, including PGS, patients can be more in control of their family-building journey. With the help of skilled healthcare providers, they can better navigate the complex world of reproductive technologies. This can lead to a successful and healthy pregnancy.
If you’d like to learn more about IVF, Egg Donation, or surrogacy services globally, check out the rest of our website at Complete Surrogacy Agency. We offer legally secure and affordable surrogacy consulting services for FREE.
Complete Surrogacy: Your Trusted Partner in International Surrogacy
At Complete Surrogacy, we have over 15 years of experience in international surrogacy, guiding 4,000+ intended parents worldwide. We provide safe, ethical, and affordable surrogacy solutions for single parents, LGBTQ+ couples, and heterosexual couples.
As members of EFS and ESHRE, we adhere to the highest ethical and professional standards. Our expert team is committed to providing accurate, compassionate, and transparent guidance, ensuring a legally secure and smooth journey to parenthood.
Let us help you build your family with trust, care, and integrity.
Get in touch for one FREE Surrogacy Consultancy!
References used:

FAQ for risks and benefits of PGS
What is PGS Testing (PGT-A)?
PGS testing, or preimplantation genetic testing for aneuploidy (PGT-A), checks embryos’ chromosomes during IVF. It looks for embryos with the right number of chromosomes. These embryos are more likely to implant well and lead to a healthy baby.
How is PGS Testing Performed?
For PGS testing, a small sample of an embryo is taken. Then, the DNA is analyzed for the right number of chromosomes. This happens at the blastocyst stage, around 5-6 days after fertilization.
Does PGS Testing Harm the Embryo?
Some worry if the embryo biopsy for PGS testing is safe. Research shows it might not harm the embryo much. But, there are also concerns about possible risks.
What are the Benefits of PGS Testing?
PGS testing could make IVF more successful and lower miscarriage risk. By choosing only embryos with the right number of chromosomes, the chance of a healthy pregnancy goes up.
What are the Limitations of PGS Testing?
PGS testing faces big challenges to work well. It needs embryos to make it to the blastocyst stage for biopsy. There are also doubts about how accurate it is, especially with embryo mosaicism.
What are the Pros and Cons of PGS Testing?
Patients and their fertility teams must think about PGS testing’s pros and cons. It might lower miscarriage risk for some, but it has big limits and risks too.
Source Links
- https://www.manchesterfertility.com/blog/preimplantation-genetic-screening-facts-benefits-risks/ – Preimplantation Genetic Screening: Facts, Benefits & Risks
- https://www.fertilityiq.com/fertilityiq/ivf-in-vitro-fertilization/pgs-genetic-screening-of-embryos – PGT-A and PGS Genetic Screening of Embryos
- https://fertility.wustl.edu/treatments-services/genetic-counseling/preimplantation-genetic-testing-faq/ – Preimplantation Genetic Testing – FAQ | Fertility & Reproductive Medicine Center
- https://crh-wp.ucsf.edu/fertility-treatment/preimplantation-genetic-testing-pgt/ – Genetic Testing (PGT & PGS) | UCSF Center for Reproductive Health

Author Bio: Neelam Chhagani is an International Surrogacy Expert with 15 years of experience in the fertility and surrogacy domain. As the founder of IVF Conceptions and Complete Surrogacy, she has guided over 4,000 intended parents worldwide on their surrogacy journey to parenthood. Recognized as a trusted authority, she specializes in holistic infertility solutions and third-party reproduction consulting.
Holding an MA in Counselling Psychology and a PGD in Mental Health, Neelam is a proud member of the European Fertility Society (EFS) and the European Society of Human Reproduction and Embryology (ESHRE). She is also a leading surrogacy blogger, providing valuable insights into ethical and practical surrogacy solutions.
Since 2010, committed to supporting ALL family types, Neelam has been passionate about helping intended parents grow their families with compassion, integrity, and a focus on secure and affordable surrogacy options Globally.
Learn more about Neelam:
https://www.ivfconceptions.com/neelam-chhagani-surrogacy-consultant/
https://www.linkedin.com/in/neelam-chhagani-92892229/












I was introduced to Neelam by a friend who worked with Neelam for surrogacy. Neelam is absolutely wonderful. I am a single male and the journey to fatherhood is not that easy. Neelam connected me to a program ideal for my circumstances. She was with me throughout the pregnancy providing advice and guidance along the way. I am so grateful I found her and am thrilled today that I have a beautiful daughter. I highly recommend Neelam to anyone who is on a journey to become a parent. Having a child has changed my world for the better. I wish others success with their own journey and recommend you connect with Neelam to find a path that is best for you.
SA (USA)